
Wilson’s disease is a rare inherited disorder that affects the body’s ability to process and eliminate excess copper. When untreated, this accumulation leads to severe damage in the liver, brain, and other vital organs. Named after Dr. Samuel Alexander Kinnier Wilson, who first described the disease in 1912, this condition requires lifelong attention but can be effectively managed with timely diagnosis and treatment.
Causes of Wilson’s Disease
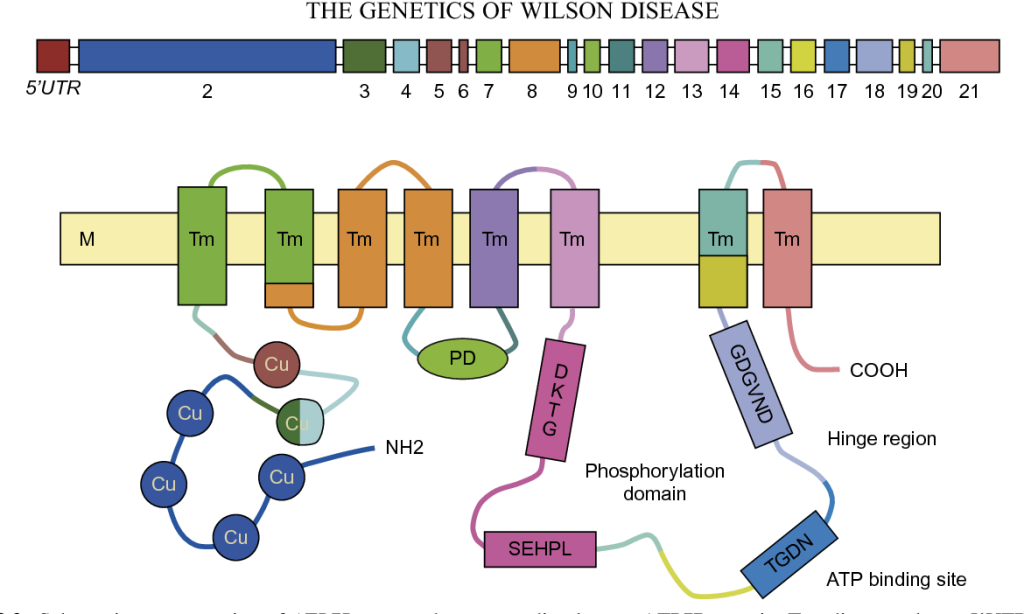
The root cause of Wilson’s disease lies in mutations of the ATP7B gene, which regulates copper metabolism. This leads to:
- Impaired Copper Excretion: The liver fails to excrete excess copper into bile.
- Tissue Damage: Copper builds up, causing toxicity in organs like the liver, brain, and eyes.
- Hereditary Nature: The condition is passed down through autosomal recessive inheritance, requiring both parents to carry the defective gene.
Indications of Wilson’s Disease
The disease’s early warning signs are often subtle and can mimic other conditions. Watch for:
- Fatigue and general weakness.
- Jaundice or yellowing of the skin and eyes.
- Behavioral changes, such as mood swings or irritability.
- Abdominal swelling or discomfort.
Symptoms of Wilson’s Disease
Wilson’s disease manifests in multiple ways depending on the organs affected:
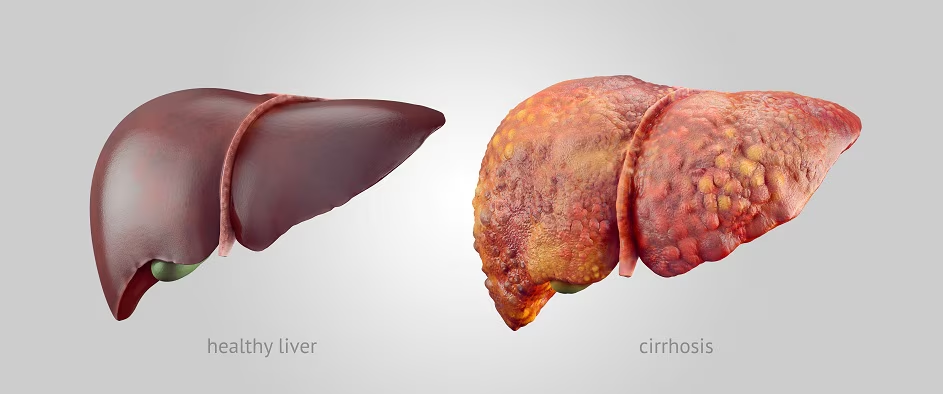
- Liver Symptoms: Chronic hepatitis, cirrhosis, or acute liver failure.
- Neurological Symptoms: Tremors, muscle rigidity, difficulty with speech or coordination.
- Psychiatric Symptoms: Anxiety, depression, or sudden personality shifts.
- Ocular Symptoms: Kayser-Fleischer rings, copper-colored deposits visible around the cornea.
Prevention Strategies of Wilson’s Disease
Though prevention of the genetic mutation isn’t possible, early detection and management can prevent complications:
- Genetic Testing: Family members of diagnosed individuals should undergo screening.
- Early Diagnosis: Regular medical evaluations and tests for high-risk individuals.
- Dietary Modifications: Avoid copper-rich foods such as shellfish, nuts, and organ meats.
- Consistent Monitoring: Routine follow-ups to track copper levels in the body.
Myths and Facts About Wilson’s Disease
- Myth: Wilson’s disease only affects adults.
Fact: Symptoms often begin in childhood or adolescence. - Myth: The disease is caused by a high-copper diet.
Fact: It is a genetic disorder unrelated to dietary copper intake. - Myth: Liver problems are the only concern.
Fact: The disease also affects the brain, eyes, and mental health.
Treatments and Therapy
Medication-Based Treatments
- Chelating Agents: Medications like penicillamine or trientine bind copper, enabling its removal through urine.
- Zinc Therapy: Blocks copper absorption from food in the digestive tract.
Surgical Treatments
- Liver Transplantation: Reserved for patients with severe liver failure unresponsive to medication.
Physical Therapy and Rehabilitation
- Helps improve motor coordination and manage tremors caused by neurological damage.
Lifestyle and Behavioral Interventions
- Adopting a copper-free diet and ensuring compliance with medications.
Alternative and Complementary Medicine
- Techniques like yoga and mindfulness can help manage stress and improve quality of life.
Psychotherapy and Counseling
- Provides emotional support and helps address psychiatric symptoms.
Immunizations and Vaccines
- Essential for individuals with compromised immune function to prevent infections.
Stem Cell Therapy
- Research is exploring its potential to repair liver damage and restore normal function.
Gene Therapy
- Offers hope for a future cure by addressing the defective ATP7B gene directly.
Top 20 FAQ on Wilson’s Disease
1. What is Wilson’s disease?
It is a genetic condition that causes toxic copper buildup in the body, leading to organ damage, particularly in the liver, brain, and eyes.
2. How is it diagnosed?
Wilson’s disease is diagnosed through:
- Physical exams.
- Blood tests (e.g., ceruloplasmin levels).
- 24-hour urine copper tests.
- Genetic testing.
- Eye examinations for Kayser-Fleischer rings.
3. What tests confirm the disease?
Tests that confirm Wilson’s disease include:
- Serum ceruloplasmin levels.
- 24-hour urine copper levels.
- Liver biopsy for measuring copper content.
4. Can it be cured completely?
While there is no cure, treatments can effectively manage the condition and prevent complications.
5. Who is at risk?
Individuals with a family history of Wilson’s disease or genetic mutations in the ATP7B gene are at higher risk.
6. Are there lifestyle changes needed?
Yes, lifestyle changes include:
- Following a low-copper diet.
- Adhering to prescribed medications.
- Regular monitoring of copper levels and organ function.
7. What are Kayser-Fleischer rings?
These are copper deposits visible around the cornea, typically detected during an eye examination and are a hallmark feature of Wilson’s disease.
8. How does it affect the brain?
Wilson’s disease can cause:
- Neurological symptoms like tremors and speech difficulties.
- Psychiatric issues such as depression, anxiety, and mood swings.
9. Can it cause infertility?
Yes, untreated Wilson’s disease may lead to hormonal imbalances that can affect fertility.
10. How is it managed during pregnancy?
Treatment continues during pregnancy with careful monitoring, often using zinc therapy, and adjusting other medications to ensure safety for both mother and baby.
11. What is the role of zinc in treatment?
Zinc reduces copper absorption in the intestines and is often used as a long-term maintenance therapy.
12. Are there home remedies?
Home remedies, such as copper-free diets and adequate hydration, can support medical treatments but cannot replace them.
13. What foods should I avoid?
Avoid foods high in copper, such as:
- Shellfish.
- Liver.
- Nuts.
- Chocolate.
- Mushrooms.
14. How long does treatment last?
Treatment is lifelong and requires consistent adherence to medications, dietary changes, and regular follow-ups.
15. What happens if untreated?
If left untreated, Wilson’s disease can lead to:
- Severe liver damage.
- Neurological impairments.
- Death.
16. Can children develop it?
Yes, symptoms can appear in children as young as five years old, though they are often diagnosed in adolescence.
17. Does it cause fatigue?
Yes, fatigue is a common symptom, primarily due to liver dysfunction and copper toxicity.
18. Is genetic testing mandatory?
Genetic testing is not mandatory but is highly recommended for families with a history of the disease to identify carriers or affected individuals.
19. Are there new treatments available?
Research into advanced therapies, including gene therapy and improved medications, is ongoing and offers hope for the future.
20. Where can I get support?
Support is available through:
- Specialized clinics for Wilson’s disease.
- Patient advocacy organizations.
- Online forums and communities for patients and caregivers.
Conclusion
Wilson’s disease, though challenging, is not insurmountable. With early diagnosis, effective treatments, and proper lifestyle changes, individuals can lead fulfilling lives. Increasing awareness and access to care can significantly improve outcomes for those living with this rare disorder. If you suspect you or a loved one may be affected, consult a healthcare provider immediately to begin your journey toward better health.
Your health is your priority—take control today!
Related video: